Introduction
Physical therapy in Ventura for Hip
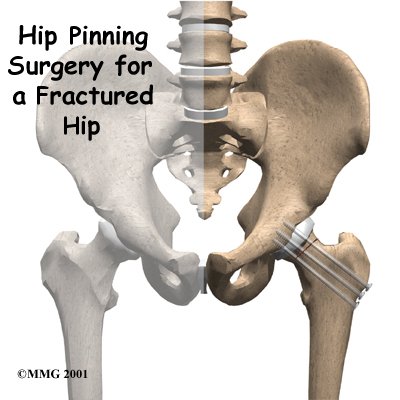
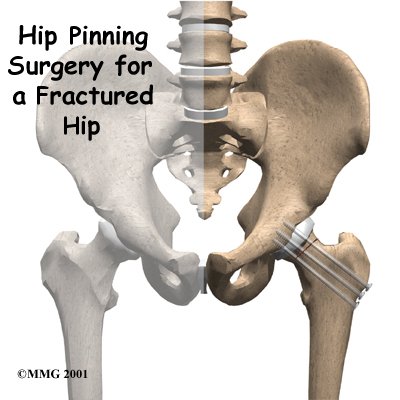
Welcome to Globerman Physical Therapy's resource with respect to recovering from Hip Pinning Surgery for a Fractured Hip.
This guide will help you understand:
- what the surgeon hopes to achieve
- what happens during the procedure
- what to expect as you recover
Related Document: Globerman Physical Therapy's Guide to Hip Fractures
Anatomy
How is the hip designed?
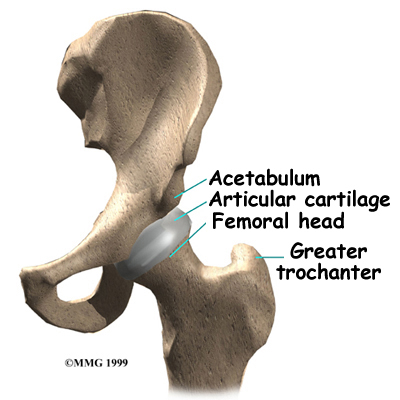
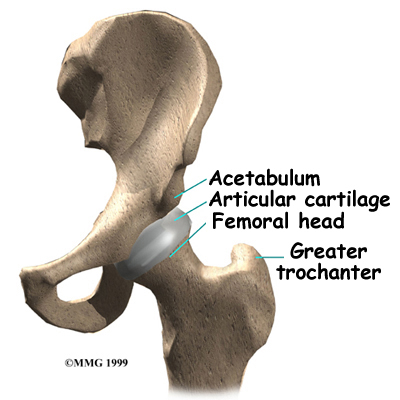
The femur is the large bone of the thigh. The ball-shaped femoral head on the end of the femur fits into a socket in the pelvis called the acetabulum. The femoral neck is a thinner part of the femur. It is the short section of bone that connects the femoral head to the main shaft of the bone. The bump on the outside of the femur just below the femoral neck is called the greater trochanter. This is where the large muscles of the buttock attach to the femur.
Hip fractures in aging adults happen either in the femoral neck or the intertrochanteric area. Fractures occur at about the same frequency for both areas.
Related Document: Globerman Physical Therapy's Guide to Hip Anatomy
Rationale
What does the surgeon hope to achieve?
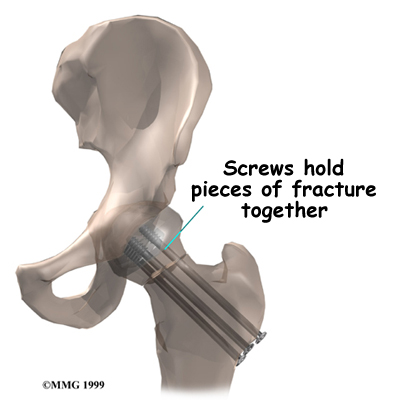
Fixing the broken ends of the hip with metal pins or screws is a fairly simple procedure. The procedure requires only a small incision on the side of the hip, and the pins and screws usually provide a solid connection for the broken bones. Patients are able to move right away after surgery, so they are more likely to avoid the serious complications that can arise with being immobilized in bed.
Most hip fractures would actually heal without surgery, but the problem is that the patient would be in bed for eight to 12 weeks. Surgeons have learned over the years that confining an aging adult to bed for this period of time has a far greater risk of creating serious complications than the surgery required to fix a broken hip. The goal of the hip pinning procedure is to set the bones securely in place, allowing the patient to get out of bed as soon as possible.
The hip pinning procedure is used successfully after most fractures within the femoral neck. When the fractured bones have displaced, however, surgeons do not all agree that the hip pinning procedure is the best choice. This is because displaced fractures can damage the blood supply going to the femoral head, leading to avascular necrosis (AVN), a condition that causes the bone of the femoral head to die. With displaced fractures, the risk of developing AVN is so high that some surgeons may suggest not fixing the fracture but instead removing the femoral head and replacing it with an artificial replacement, or prosthesis. This is suggested because pinning the fracture carries a high chance that you will need a second operation several months later if the femoral head dies due to AVN.
Related Document: Globerman Physical Therapy's Guide to Avascular Necrosis of the Hip
Preparation
How should I prepare for surgery?
The hip pinning procedure is usually an emergency surgery, so it is unlikely that you will have had time to plan and prepare. Ideally a caregiver, such as a family member or friend, will help make arrangements for you while you are in the hospital.
The surgeon and care team will communicate with your caregiver to help with these preparations. Your caregiver will help coordinate your ride home, make sure you have needed supplies, and set up follow-up appointments with your surgeon, doctor, and physical therapist.
Surgical Procedure
What happens during the operation?
The operation can be done using either a general anesthetic (one that puts you to sleep) or a spinal block. The spinal block puts your body to sleep from the waist down. With a spinal block, the anesthesiologist will also give you medications so that you won't be aware the operation is being done.
Once you have anesthesia, your surgeon will make sure the skin of your hip is free of infection by cleaning the skin with a germ-killing solution.
With the patient lying flat on a special table, the foot and leg are supported. Tension is applied to get the fractured bones to line up. The surgeon checks the alignment using a fluoroscope, a type of X-ray machine that shows the image on a TV screen.
A small incision is made on the side of the thigh. The surgeon uses the fluoroscope to guide the metal screws or pins into the correct position to hold the bones together. The fluoroscope allows the surgeon to see the X-ray image of the hip while the screws are placed through the femoral neck.
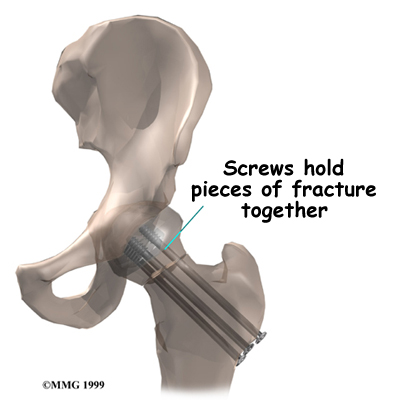
The soft tissues are put back in place, and metal staples or sutures are used to close the incision.
Complications
What might go wrong?
The main complications after a hip fracture sometimes develop as a result of being immobilized in bed. These may include pneumonia, bedsores, and mental confusion.
Complications that can result from the hip pinning surgery itself include:
- anesthesia complications
- thrombophlebitis
- infection
- nerve or blood vessel injury
- avascular necrosis of the femoral head
- nonunion of the bones
This is not intended to be a complete list of possible complications.
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but it is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include:
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Any surgery carries the risk of infection. You will probably be given antibiotics before the procedure to reduce the risk. If you get an infection, you will need more antibiotics. If the areas around the metal pins or screws become infected, you may need surgery to drain the infection.
Nerve or Blood Vessel Injury
Several nerves and blood vessels travel in the area where the surgery is performed. It is possible to injure either the nerves or the blood vessels during surgery, but this is extremely unlikely during this type of surgery. Nerve problems may well be temporary if the nerves have been stretched by retractors holding them out of the way. It is rare to have permanent injury to either the nerves or the blood vessels, but it is possible.
Avascular Necrosis (AVN)
As described earlier, all of the blood supply comes into the ball that forms the hip joint through the neck of the femur bone. If this blood supply is damaged, there is no backup. Damage to the blood supply can lead to the bone that makes up the ball portion of the femur actually dying. Once this occurs, the bone is no longer able to maintain itself. When the neck of the femur fractures, the blood supply may be damaged, leading to problems with avascular necrosis. The risk of AVN is much higher when the fracture causes a large displacement in the bones. AVN can show up as late as two years after the surgery.
Related Document: Globerman Physical Therapy's Guide to Avascular Necrosis of the Hip
Nonunion
Sometimes the bones do not bond together as planned. This is called a nonunion, or pseudarthrosis. This condition requires another operation to add more fixation or actually replace the head of the femur, a procedure called hemiarthroplasty.
Related Document: Globerman Physical Therapys Guide to Hemiarthroplasty of the Hip
After Surgery
What happens after surgery?
After surgery, your hip will be covered with a padded dressing. If your surgeon used a general anesthesia, a nurse or respiratory therapist will guide you in a series of breathing exercises. You'll use an incentive spirometer to improve breathing and avoid possible problems with pneumonia.
A physical therapist will direct your recovery after surgery. You'll be encouraged to move from your hospital bed to a chair several times the first day after surgery. You'll be encouraged to begin getting up and walking with your crutches or walker but may need to keep from placing too much weight on your foot while you stand or walk. You'll be safe to go home when you can get up and move about safely with your walker or crutches, you are able to do your exercises, and your caregiver has made all the needed preparations for you to go home.
After surgery, you should keep the dressing on your hip until you return to the surgeon. Avoid getting the stitches wet. Your stitches will be removed 10 to 14 days after surgery. You should support your outer hip with a pillow when you sit or recline.
Portions of this document copyright MMG, LLC.
Our Rehabilitation
What should I expect during my recovery?
Once discharged from the hospital, your Globerman Physical Therapy physical therapist may see you for in-home treatments. This is to ensure you are safe in and about the home and getting in and out of a car. Our physical therapist will make recommendations about your safety, review your exercise program, and continue working with you on walking and strength. In some cases you may require additional visits at home before beginning our outpatient physical therapy. Home therapy visits end when you are safe to get out of the house.
Additional outpatient physical therapy visits are sometimes needed for patients who still have problems walking or who need to get back to physically heavy work or activities.
Our therapist may use hands-on stretches for improving range of motion. Then we use strength exercises to address key muscle groups including the buttock, hip, and thigh. Endurance can be achieved through stationary biking, lap swimming, and using an upper body ergometer (upper cycle).
Globerman Physical Therapy physical therapists sometimes treat patients in a pool. Exercising in a swimming pool puts less stress on the hip joint, and the buoyancy allows you to move and exercise easier. Once you've gotten your pool exercises down and the other parts of your rehab program advance, we may instruct you in an independent program.
When you are safe in putting full weight through the leg, our physical therapist will choose several types of balance exercises to further stabilize and control the hip.
Finally, we can use a select group of exercises to simulate day-to-day activities, such as going up and down steps, squatting, and walking on uneven terrain. Specific exercises may then be chosen to simulate work or hobby demands.
At Globerman Physical Therapy, our goal is to help you maximize hip range of motion and strength, restore a normal walking pattern, and do your activities without risking further injury to the hip. When your recovery is well under way, regular visits to our office will end. Although we will continue to be a resource, you will be in charge of doing your exercises as part of an ongoing home program.
Globerman Physical Therapy provides services for physical therapy in Ventura.